Posterior nasal packing
Nasal packing is a second-line therapy. See Epistaxis for more guidance.
This page is for reference, not instruction: you should be shown how to do this by a senior before attempting it on your own.
INDICATIONS
Bleeding is not controlled by adequate bilateral anterior nasal packing
High clinical suspicion of a posterior bleed:
Blood initially at the back of the mouth
Bilateral profuse bleeding
Previous posterior bleed
But remember that posterior bleeds are rare
A posterior nasal pack aims to produce choanal obstruction and tamponade along with anterior packing. It is always placed with anterior packing. Some manufacturers produce double-balloon inflatable packs which are simpler to insert (Rapid Rhino 900® or Invotec Ultra Stat®). Posterior packing with a Foley catheter is still felt by many surgeons to be the go-to temporising measure in severe epistaxis.
PREPARATION
Reassure the patient: severe epistaxis is frightening for the patient
You should have discussed this case with the ENT Registrar
Get assistants and all the equipment you need: do not settle for less
Explain the necessity of placing a posterior pack to the patient and the sensation of pressure or foreign body at the back of the nose, as well as a pressure headache
Equipment
Wall suction and Yankauer catheters
Headlight
Thudichum’s speculum
12F or 14F Foley catheters
Cotton wool
Tilley's nasal dressing forceps
Scissors
10ml Syringes
Aqueous gel lubrication
Umbilical cord clamp/ tubing clamp
Gauze swabs
Disposable sick bowls
Tissues
Glass of water
Co-phenylcaine ( 5% lidocaine and 0.5% phenylephrine)
Anterior packing options: Rapid Rhino®, Merocel®, bismuth iodoform paraffin paste (BIPP) impregnated ribbon gauze etc.
Look after yourself and your colleagues: everyone must wear visor mask, apron and gloves.
Before you continue you must prepare the Foley catheter:
Check the balloon by inflating with 10ml air
If desired, trim the tip of the catheter without bursting the balloon: this is more comfortable for the patient
Deflate the balloon
Silicone Foley catheter with inflated balloon
INSERTION
Place the patient in an upright position
Suction the nose as best you can
Have your assistant(s) continue to apply suction to the pharynx or nose while you are working
Spray the nasal passages with co-phenylcaine or apply with soaked cotton pledgets
Use a small amount of lubrication on the tip of the Foley catheter.
Insert the Foley catheter into the side that is thought to be bleeding, directly horizontally along the floor of the nose towards the ipsilateral earlobe
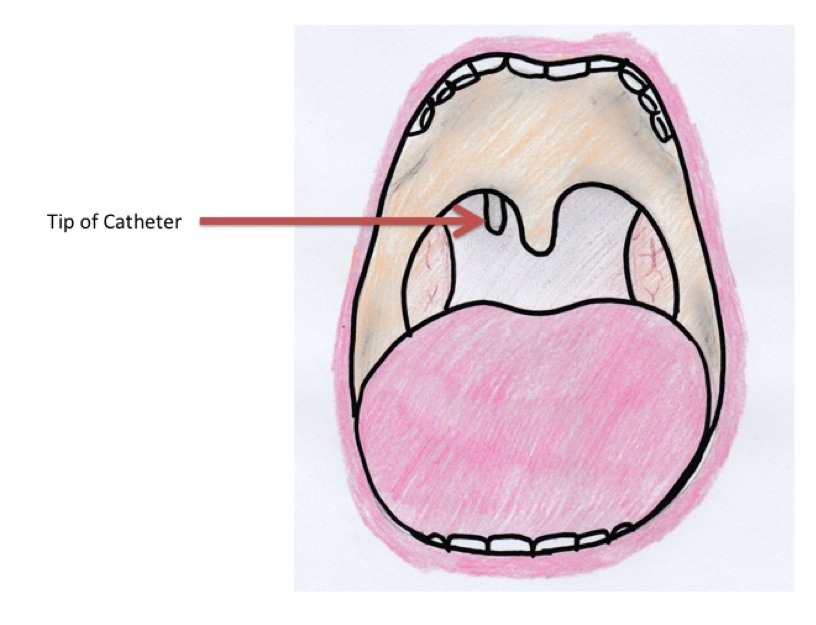
Ask the patient to keep their mouth open as you advance the Foley catheter until you see the tip dangling into the oropharynx
When you see the tip of the Foley catheter, inflate the balloon
Aim to fill with 10ml air * but do not exceed what the patient is able to tolerate
Pull the catheter firmly forwards: the balloon should be pulled against the choana; this will hurt
Ask your assistant to maintain tension on the Foley catheter while you proceed with bilateral anterior packing eg Rapid Rhinos
While exerting firm traction, secure the Foley catheter with an umbilical clip (or tubing clamp) at the nostril to prevent the catheter slipping back
YOU MUST place a wad of gauze or other padding between the clamp and the skin of the nose, as prolonged contact causes pressure necrosis and a hard-to-reconstruct aesthetic deformity
The catheter should be secured to the patient's face with tape
Insert along the floor of the nose
Look inside the oropharynx for the tip of the catheter
For petroleum jelly- or BIPP-impregnated ribbon gauze:
Materials can be found in ENT theatres: you can usually obtain packets of ribbon gauze pre-impregnated with BIPP or petroleum jelly but make sure you have long ribbons (most surgical ribbon gauze comes in packs of 1.25m x 1m)
Hold one end of the ribbon outside the nose and layer a loop along the floor of the nose right to the back
Then release your Tilley's and then lay another loop on top of this and repeat until the nose is full
Cut the ribbon and ensure both ends are secured to the face
Be warned that this is an incredibly uncomfortable procedure for the patient
NB If a fluoroscopic embolisation is planned, do not use X-Ray detectable ribbon gauze or BIPP as both will cause significant artefact: we strongly recommend the use of inflatable or tampon packs instead
CHECK YOUR HAEMOSTASIS
To ensure adequate haemostasis, ask the patient to gargle and spit water to clean the back of the throat, then look for any ongoing bleeding in the oropharynx.
PROBLEMS
Bleeding continues
Is the posterior pack properly sited?
Are all balloons adequately inflated?
Is there still traction of the Foley catheter forwards? If not, you can layer more gauze wadding between the cord clamp and the nostril
Are the anterior packs adequate?
You should discuss all further bleeding with the ENT Registrar, as your patient is likely to need to go to theatre for surgical management (e.g. SPA ligation).
Repeated posterior packing should not be undertaken without discussion with a senior. Patients requiring and/or failing posterior packing need SPA ligation unless there are contraindications.
IN PARALLEL (USE YOUR ASSISTANTS)
Full history and ABCDE assessment
Secure wide bore IV access and send FBC, U&E, coagulation screen/INR and G&S (+/- fibrinogen and D-dimer if indicated)
Be aware of coagulopathy and discuss with the appropriate specialties:
Is it a primary coagulation or platelet disorder?
Is it disseminated intravascular coagulopathy (DIC) - is the patient septic, or had major surgery or trauma, or is there active cancer?
For anticoagulated patients with severe bleeding, you should discuss the need for rapid reversal of anticoagulation or conversion to unfractionated heparin.
Always prescribe analgesia - your patient is in significant discomfort
If analgesia is not effective, discussion with a senior or anaesthetist, a small dose of benzodiazepine may be warranted
Prescribe broad spectrum antibiotics to reduce the chances of sinusitis/toxic shock syndrome.
Admit to an ENT ward
Packs are likely to need to stay in for >24 hour
Talk to your patient about the plan and reassure them - this is emotionally and physically traumatic
* We recommend air for the Foley catheter as 1) it is being used as an airway device; 2) the pressure applied is more consistent; 3) there is less confusion since air is also used for Rapid Rhino packs.
Page last reviewed: 9 December 2019