Septal Haematoma
Red Flags
Septal abscess formation with features including increasing pain, fever and purulent nasal discharge.
If there is a history of trauma, ensure other injuries are excluded.
Why is this important?
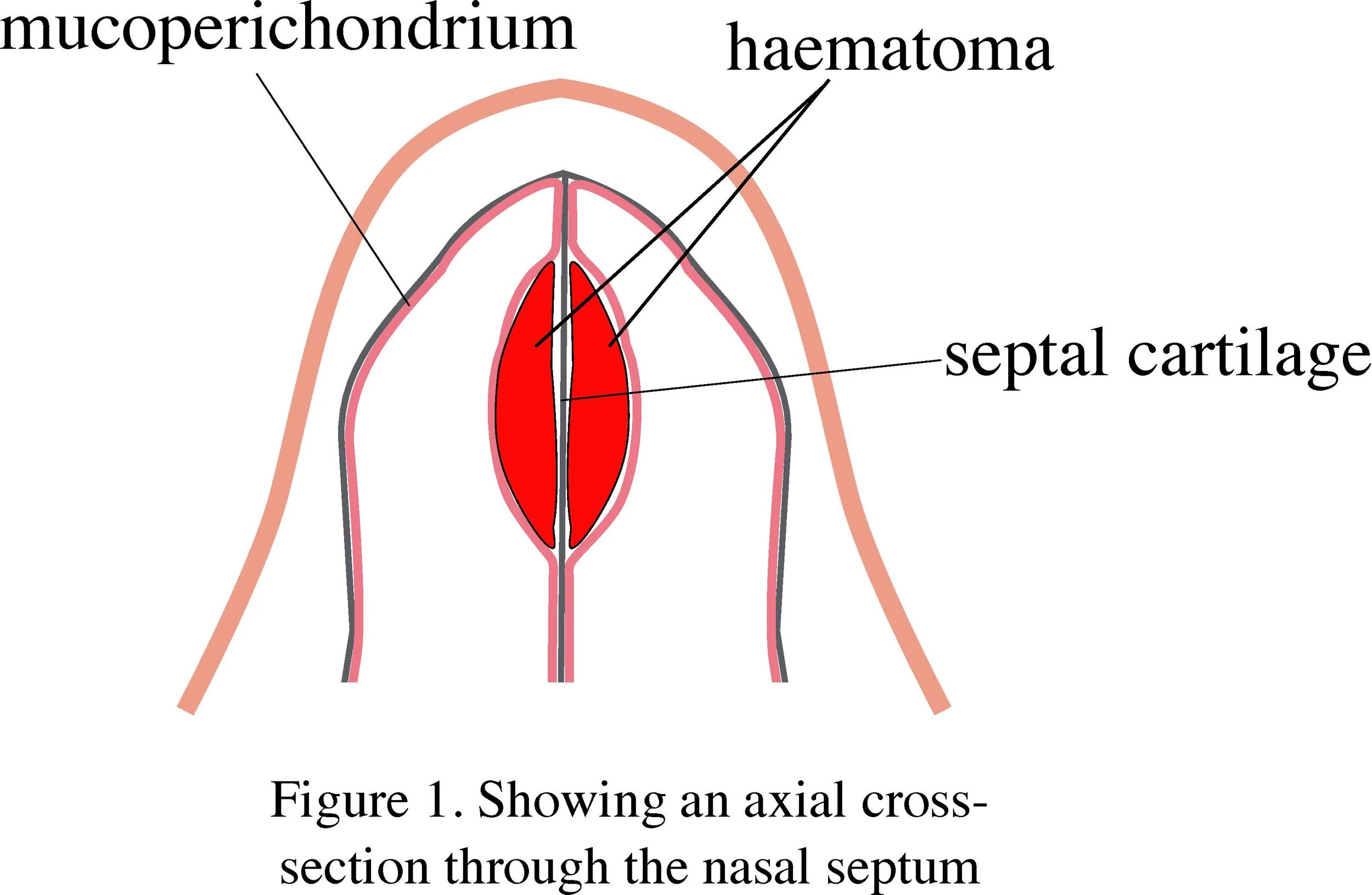
The blood supply runs within the mucoperichondrium surrounding the septal cartilage. Shearing forces from trauma tear these vessels and a septal haematoma forms in the potential space between the two layers (Figure 1). This can result in avascular necrosis of the cartilage and possible formation of a septal abscess through secondary infection.
Loss of a substantial amount of septal cartilage can lead to a permanent septal perforation, and/or saddle nose deformity. Rarely, a septal abscess can spread intracranially via the venous drainage of the mid-face, leading to cavernous sinus thrombosis
Figure 1.
When to involve the ENT registrar
Discuss any patient with a suspected haematoma
Discuss all cases of septal abscess or suspected intracranial extension
Who to admit
All patients with a septal haematoma should be admitted as they will require drainage of the haematoma +/- nasal packing to prevent re-accumulation of the haematoma +/- intravenous antibiotics, depending on the situation.
Assessment and recognition
Septal haematoma should be excluded in any patient presenting with a history of facial or nasal trauma. Suspect a haematoma if the patient presents after an injury with bilateral nasal blockage and/or pain. Some patients can present in a delayed fashion.
A full nasal examination should be performed, along with a holistic assessment of other injuries using the ATLS approach, alongside the designated trauma team.
Septal haematomas most commonly occur in the anterior portion of the septum and appear as a red, usually bilateral swelling (see YouTube link below.) NB: A septal haematoma is not simply the presence of blood clots in the nasal passages)
If in doubt as to the nature of the swelling, the mass can be palpated with a gloved finger or a blunt instrument such as a microbiology swab; a haematoma feels soft and fluctuant whereas a deviated nasal septum will be firm and will be concave on the opposite side
A definitive diagnosis can be achieved by needle aspiration: a bloody or serosanguinous aspirate is a positive finding; this is generally done by spraying the nose with local anaesthetic spray and aspirating with a 10ml syringe and green needle
Immediate and overnight management
A septal haematoma should ideally be drained within hours of presentation, as necrosis can occur within 24 hours. Initial aspiration with a wide bore needle may confirm the diagnosis, but has a high rate of reaccumulation.
Discuss management with a senior, as most patients require incision and drainage under general anaesthesia.
In cases of suspected infection, send a swab/aspirate for M,C+S. All septal abscesses require incision and drainage under general anaesthesia.
Following drainage, through-and-through dissolvable sutures may be placed into the septum. Many surgeons also pack the nose to prevent re-accumulation of the haematoma. Patients may be started on antibiotics to minimise the risk of secondary infection.
For reference, here is a video on incision and drainage (starts at 03:10).
Further management
Patients who have had an I&D under general anaesthesia would normally have bilateral nasal packs +/- a corrugated drain placed in between the mucoperichondrial layer and the nasal septum. These typically stay in for 36-48 hours and the patients can be placed on antibiotics.
Patients who have had repeated haematomas or a septal abscess are high risk for septal perforation and saddle deformity.
It is best that all patients who have had a septal haematoma drained be followed up in the main outpatients clinic in 2-3 weeks.
References
Kass JI, Ferguson BJ. Treatment of Hematoma of the Nasal Septum. N Engl J Med [Internet]. Massachusetts Medical Society; 2015 May 28 [cited 2016 Oct 4];372(22):e28. Available from: http://www.nejm.org/doi/abs/10.1056/NEJMvcm1010616
Alshaikh N, Lo S. Int J Ped Otorhinolaryngol. Nasal septal abscess in children : From diagnosis to management and prevention. Int J Pediatr Otorhinolaryngol [Internet]. Elsevier Ireland Ltd; 2011;75(6):737–44. Available from: http://dx.doi.org/10.1016/j.ijporl.2011.03.010
Canty PA, Berkowitz RG. Hematoma and abscess of the nasal septum in children. Arch Otolaryngol Head Neck Surg [Internet]. 1996 Dec [cited 2016 Oct 2];122(12):1373–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8956753
Page last reviewed: 1 December 2022