Audiometry
A basic understanding of audiometry is an important skill to have as hearing loss is a common referral to the on-call SHO as well as in the outpatient department.
Hearing loss can be categorised into conductive (problems with sound reaching the auditory nerve), sensorineural (problems with the auditory nerve itself), or mixed.
In this article we describe how to assess patients with hearing loss and interpreting common audiological tests.
Common audiological tests
Tuning fork tests
These are basic bedside screening hearing assessment tools, most useful with a 512Hz tuning fork.
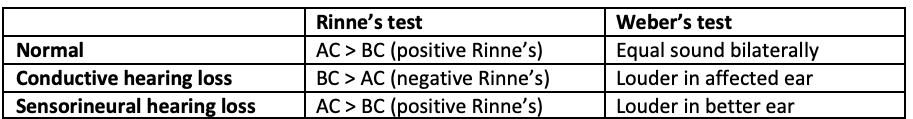
Interpreting the results of Rinne’s and Weber’s tests together help form a diagnosis.
Rinne’s test: comparing air and bone conduction
Place the ringing tuning fork over the patient’s mastoid process
Then place the tuning fork in line with their ear canal
Ask the patient if the sound is louder in front of the ear, behind, or the same in both
Positive Rinne’s means air conduction is better than bone conduction (AC>BC) = normal hearing OR sensorineural hearing loss
Negative Rinne’s means BC>AC, in other words that there is a conductive hearing loss
Weber’s test: tests bone conduction and lateralization of sound
Place the ringing tuning fork in the midline of the patient’s forehead
Ask if they hear it louder in one ear, or equally in both
Normal hearing: sound heard equally
Unilateral conductive hearing loss: sound heard louder in the affected ear
Unilateral sensorineural hearing loss: sound heard louder in the better ear.
Pure-tone audiometry
Pure-tone audiometry (PTA) or audiograms are subjective tests usually performed by audiologists in clinic. They are useful at determining the type AND severity of hearing loss.
As an overview, this tests both air and bone-conduction using earphones or bone oscillators. Hearing is tested at frequencies of 125 to 8000Hz and intensities of 10 to 110dB.
Tympanometry
Tympanograms are an objective test of middle-ear function.
Sound transmission from the external to the middle ear is optimal when the pressures in the ear canal and middle ear are equal. Tympanograms measure the compliance of the tympanic membrane, and therefore measure middle-ear pressure indirectly.
Compliance is measured by how much sound is reflected by the tympanic membrane at different air pressures from -200 mmH2O to +200 mmH2O / daPa.
A detailed description of how these tests are performed is given by the British Association of Audiologists here.
Contra-indications
Patients unable to co-operate e.g. very young age, learning difficulties, neurological impairment etc.
Clear external ear pathology e.g. wax or infection – treat this first
Interpreting audiograms and tympanograms
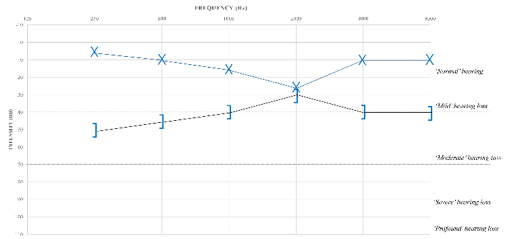
Audiograms
Read the audiogram from left (lowest pitch) to right (highest pitch)
The higher the dB level for each frequency, the worse the hearing
Assess whether the hearing is normal, sensorineural or a conductive loss in each ear
Example audiogram: Normal air conduction bilaterally; bone conduction not performed.
Tympanograms
Tympanograms tell us the compliance of the tympanic membrane (y-axis) and the ear-canal volume (space under the line / volume). Volume is often calculated for you, in ml or cm3.
Graph shapes are classified into Jerger classification types:
Type A: normal.
Peak compliance is at 0mmH2O, ranging -100 to +200.
Shallow peaks (As) represent restricted TM movement e.g. otosclerosis
High/deep peaks (Ad) represent hyper-compliance e.g. ossicular disarticulation.
Type B: flat.
Normal ear-canal volume (0.3-2ml): usually middle ear effusion
High ear-canal volume: usually TM perforation
Type C: low pressure in the middle-ear
Eustachian tube dysfunction.
Case-based discussions
Case 1
A 3-year-old child is seen in clinic with speech delay and difficulty hearing teachers at school.
Audiogram: Right-sided conductive hearing loss
Tympanogram: Jerger Type B with normal ECV
Diagnosis: Right otitis media with effusion (glue ear).
Case 2
An 80 year-old patient is brought to clinic by their partner, complaining that they have the TV volume on too high.
Audiogram: Bilateral mild to severe sensorineural hearing loss, worst at higher frequencies.
Tympanogram: Jerger Type A
Diagnosis: Bilateral presbyacusis (age-related hearing loss).
Case 3
A 25 year-old female attends with muffled left sided hearing, with a family history of hearing loss.
Audiogram: Left conductive hearing loss with a reduction in air-bone gap at 2000 Hz (Carhart’s notch)
Tympanogram: Jerger Type As (shallow)
Diagnosis: Left-sided conductive hearing loss; possible otosclerosis
Page last reviewed: 8 January 2024