Tonsillitis
Red flags
Red flags
Severe sore throat, hoarse/croaky voice, severe dysphagia and fever is epiglottitis until proven otherwise. Stridor may be a late sign and patients can decompensate rapidly.
Beware of severe sore throat with severe dysphagia - without any signs of tonsillitis/pharyngitis in the oropharynx. You should rule out epiglottitis first.
Trismus (reduced mouth opening), 'hot potato' voice and stertor (snoring sound of pharyngeal obstruction) point to a peritonsillar abscess or quinsy.
Why is this important?
Although rare, epiglottitis can present with sore throat as the primary symptom so it is important to have a high index of suspicion.
It's important to recognise quinsies as they usually need aspiration.
Sore throats and tonsillitis are very common.
When to involve the ENT Registrar
Immediately: If you suspect that you may be dealing with epiglottitis, see stridor for immediate management.
Who to admit
Admit anyone unable to swallow at least a few sips of fluid regularly
Patients with stertor
Patients with a quinsy (if they can swallow good amounts after aspiration of pus, it would be reasonable to discharge after a few hours)
Important: sore throat, malaise, lymphadenopathy etc. are expected symptoms of tonsillitis and, if the person can still swallow good amounts of fluid, would not normally prompt admission
Important: many patients have not had adequate analgesia before presentation, so it's a good idea to try good oral pain relief first before reassessing whether they can cope at home, with admission as a safety net.
Photo: Normal adult oropharynx. Note the position of the anterior arches in relation to the tonsils, which are bilaterally small as expected.
Assessment and recognition
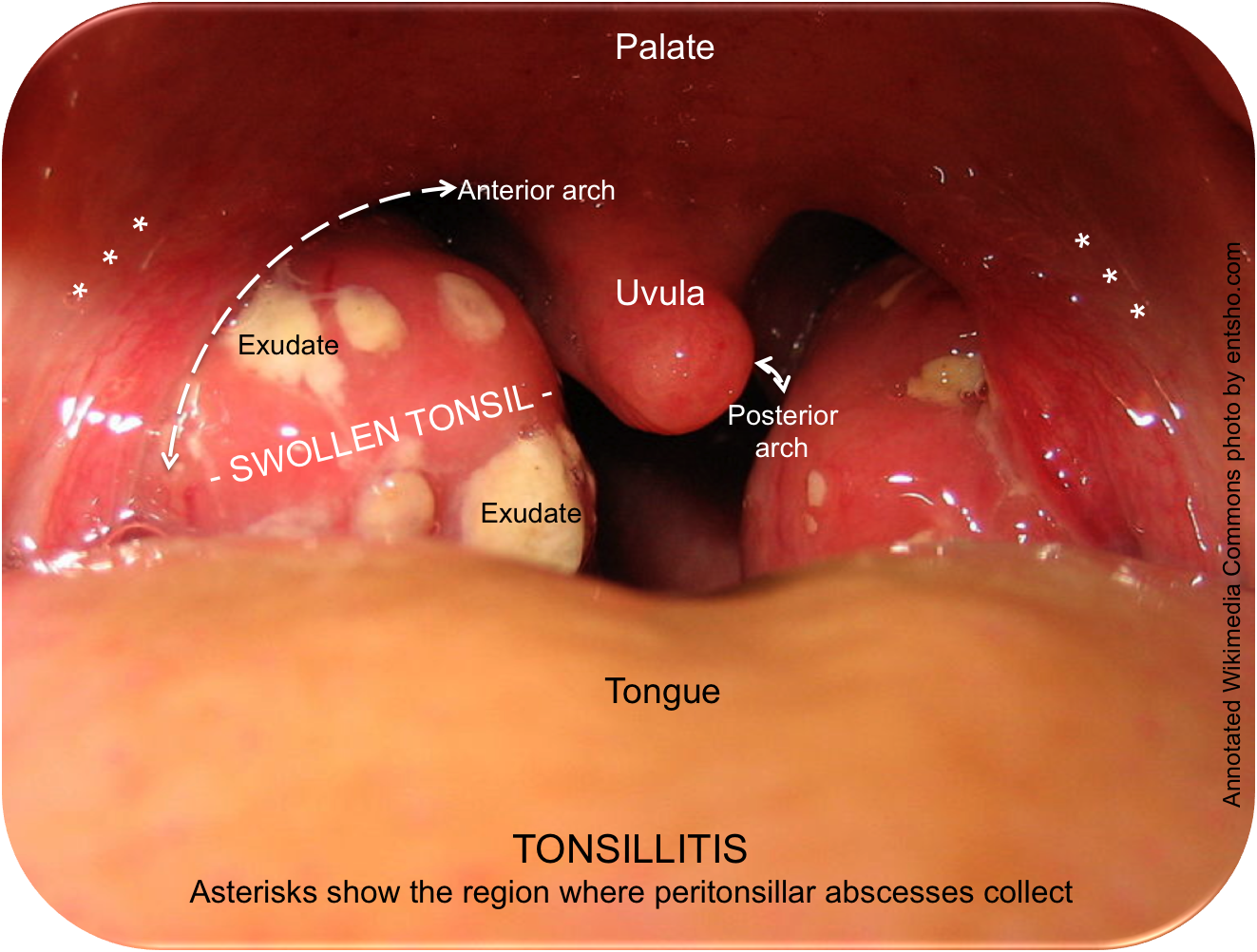
Photo: Tonsillitis. Note that the anterior arches have not changed their positions relative to the (now swollen) tonsils: note also where a quinsy would collect, causing the palate and arch to move medially.
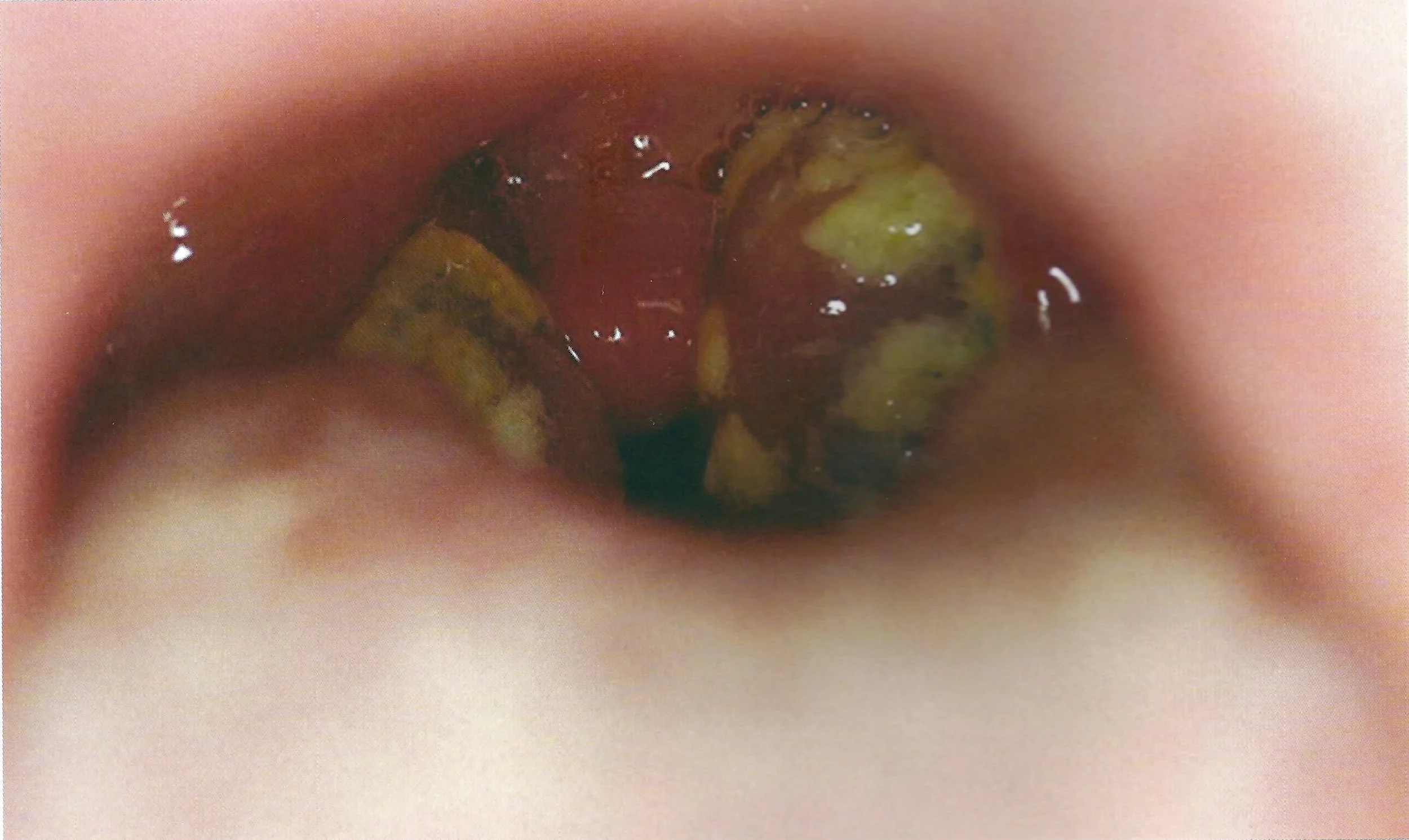
Photo: Tonsillitis in a different patient. Note the exudate on both sides and the position of the anterior arches.
Odynophagia
Dysphagia
Anorexia
Pyrexia
Malaise
Swollen tonsils with or without exudate
'Thick' or 'hot potato' voice (not hoarse voice)
Lymphadenopathy (especially Level II/III)
Referred otalgia (the glossopharyngeal nerve has a tympanic branch)
Carefully take a history and examine the patient.
Patients with pain predominantly on one side, trismus (reduced mouth opening) and a hot-potato voice may have a peritonsillar abscess.
A swollen tonsil is NOT a peritonsillar abscess (quinsy). Clarification on the clinical features of peritonsillar abscess can be found here.
Immediate and overnight management
Sore throats are common, most are viral and few present to secondary care. Antibiotics are unlikely to help with the majority of sore throats.
In many low-risk cases, it is reasonable to give a delayed or no prescription, plenty of analgesia and safety netting. This is recommended in NICE Clinical Guideline 69.
You may want to score patients for the likelihood of having a bacterial tonsillopharyngitis.
In patients who present to A&E or a walk-in centre, it is possible to avoid admission in a majority of patient with immediate administration of good analgesia (see below), IV fluids, and a single shot of IV antibiotics and steroid. After an hour or two, many patients are well enough to leave with a prescription for analgesia and antibiotics.
Suggest a brief admission to patients who cannot swallow fluids after this initial management. Some patients require overnight admission; usually patients are discharged the following morning.
Be wary of patients with stertor (the snoring sound of pharyngeal obstruction). While stertorous patients very rarely become hypoxic, it would be sensible to admit the patient for observation whilst initial treatment takes effect. Nurse the patient semi-erect and have suction available.
A good starting point when admitting patients:
IV access
FBC, U&Es, LFTs, glandular fever screen (serology or heterophile antibody test depending on policy)
Regular basic IV/PO analgesia: paracetamol and ibuprofen with stronger PRNs (NB: codeine is contraindicated in under-18s).
Topical analgesic spray e.g. benzydamine spray.
Fluid resuscitation - the vast majority of patients are young and dehydrated, and 1L of normal saline given over 1-2 hours is very effective.
A single stat dose of steroid (e.g. 6.6mg dexamethasone sodium phosphate IV, or 40mg prednisolone PO) can help, especially in those who have stertor. There is good evidence that a single dose of steroid improves recovery in primary care (Cochrane Review), but not in secondary care.
It may be difficult to examine the oropharynx if there is significant trismus. This raises the suspicion of peritonsillar abscess (quinsy). In this case, it's reasonable to admit the patient, give them some IV medication and re-examine later. The initial treatment can improve your view.
Abscesses need aspiration or I&D and, if trismus is not too much of a problem, early intervention brings significant relief.
management of recurrent tonsillitis
Tonsillitis and quinsy can disrupt school and working life significantly. In the UK, something like 35 million days are lost annually to sore throats (ENT UK 2009). Here are some consensus statements for offering tonsillectomy:
ENT UK Commissioning Guide for Tonsillectomy (2021)
Scottish Intercollegiate Guidelines Network (SIGN) 117: Indications for Tonsillectomy (2010)
Page last reviewed: 18 January 2026