Acute Sore Throat
TRIAGE QUESTIONS
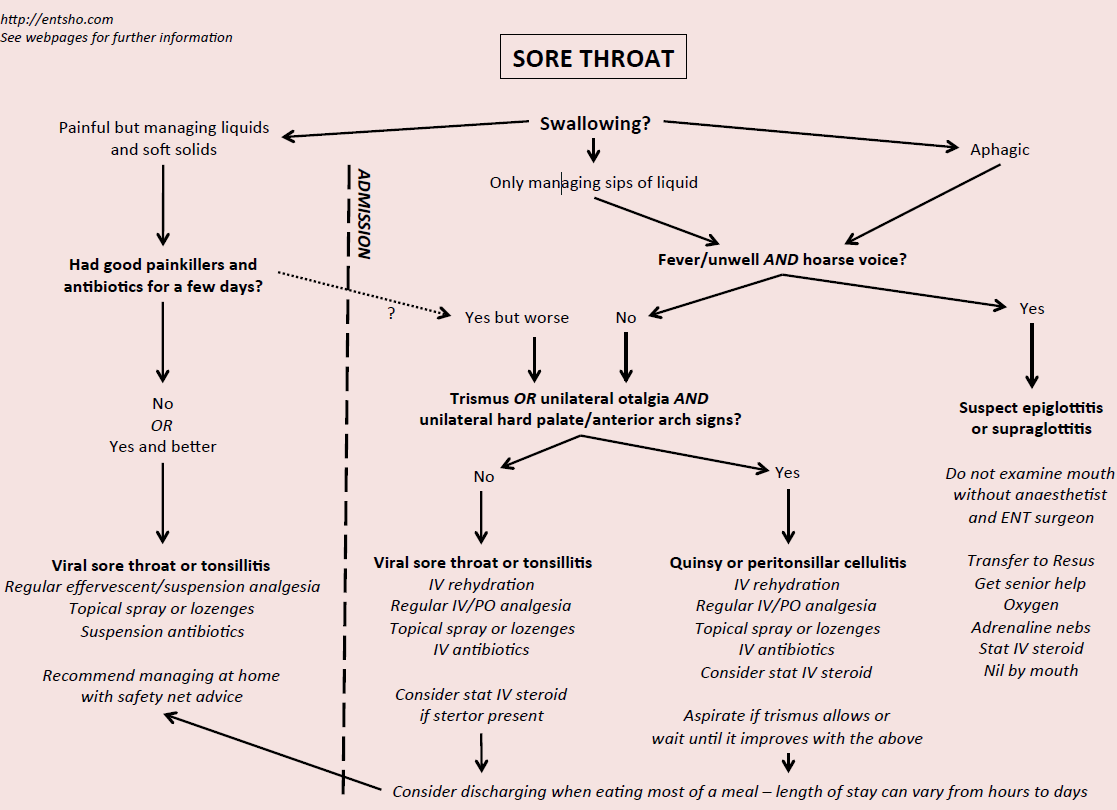
Question 1: What can the patient swallow?
Odynophagia with absolute aphagia implies admission for fluid and antibiotic therapy, regardless of diagnosis; note that patients who cannot swallow their own saliva will drool or spit
Absolute aphagia is rare and should make you suspicious that there is a serious illness
Patients able to swallow saliva and small sips of fluid may do alright at home if this is the first visit and they have not had any medication yet; equally, patients struggling despite a few days of analgesia and rest may need admission
Patients able to swallow good amounts of fluid and a small amount of soft diet should be managed at home
Odynophagia with severe dysphagia or absolute aphagia suggests a very severe tonsillopharyngitis, peritonsillar abscess or epiglottitis
Odynophagia with moderate dysphagia suggests tonsillopharyngitis or glandular fever/viral sore throat
Question 2: Is there voice change?
Hoarse, weak or croaky voice (as if they had been shouting themselves hoarse) is a worrying sign of epiglottitis or a deep neck space abscess
'Hot potato' or snoring voice (like someone with a low GCS or doing a Mr Bean impression) suggests pharyngeal inflammation from a severe tonsillitis or peritonsillar abscess
Question 3: Is there trismus?
Limitation of mouth opening implies a collection of pus causing muscle spasm, usually present in peritonsillar abscess, dental abscess and deep neck space abscess
Overuse of antibiotics is a massive problem: please calculate the Centor score before you consider prescribing them! The majority of sore throats are viral and self-limiting.
Remember, hoarseness with severe sore throat and dysphagia should set your Spidey sense tingling.
Moderate to severe unremitting (usually unilateral) sore throat for three weeks or more is a red flag symptom for urgent outpatient referral on the suspected cancer pathway.
TRIAGE FLOWCHART
To download the PDF version of this flowchart, please click on the image.
Page last reviewed: 1 December 2022